On 20 August 2025, a pregnant woman in Bulape, a rural community in Kasai province, about a thousand kilometres from Kinshasa, capital of the Democratic Republic of Congo, presented at the local General Reference Hospital with high fever, bloody diarrhoea, haemorrhage and extreme weakness. She died five days later from multiple organ failure, and what initially appeared to be an isolated tragedy has escalated into a national health security concern.
The Ebola Virus Disease is a deadly infectious disease with a fatality rate of up to 90%. Outbreaks often begin when the virus is transmitted to humans through close contact with infected wildlife, after which it spreads from person to person through direct contact with blood or bodily fluids. A single case can escalate into a large outbreak, especially if there are delays in detection and isolation, as the virus spreads from person to person. When patients with Ebola are admitted to hospitals, where the disease is not initially suspected, facilities can become amplification points. In such cases, when healthcare workers are among the infected or dead, it serves as a critical warning sign.
The Ebola virus was first identified in 1976, and has re-emerged several times in Africa, but the 2014-2016 outbreak in West Africa remains the largest to date. It affected Guinea, Liberia, and Sierra Leone, resulting in more than 28,600 reported cases and 11,325 deaths. The virus spread to seven additional countries, and in August 2014, the World Health Organization (WHO) declared Ebola a Public Health Emergency of International Concern. The scale of the outbreak overwhelmed health systems in the three hardest-hit countries and exposed major gaps in Africa’s pandemic preparedness and response strategies.
However, since that outbreak, many African countries have strengthened their health security infrastructure. Health care workers are now better trained to recognise Ebola, apply infection prevention and control measures, and manage cases when they occur. Several countries have established national public health agencies and strengthened their workforce, while tools such as vaccines and therapeutics have become available to prevent and manage cases.
As of 10 September 2025, the outbreak in Kasai province has resulted in 32 suspected cases, 20 confirmed cases, and 16 deaths. Even though the index patient was a pregnant woman in Bulape, efforts are now focused on identifying all infected patients, and tracing their contacts to curb further spread. The rural nature of the affected region poses both challenges and opportunities, while access makes it very difficult for first responders to reach communities quickly, it also limits the ability of infected individuals to travel far beyond the region.
Response from WHO and partners
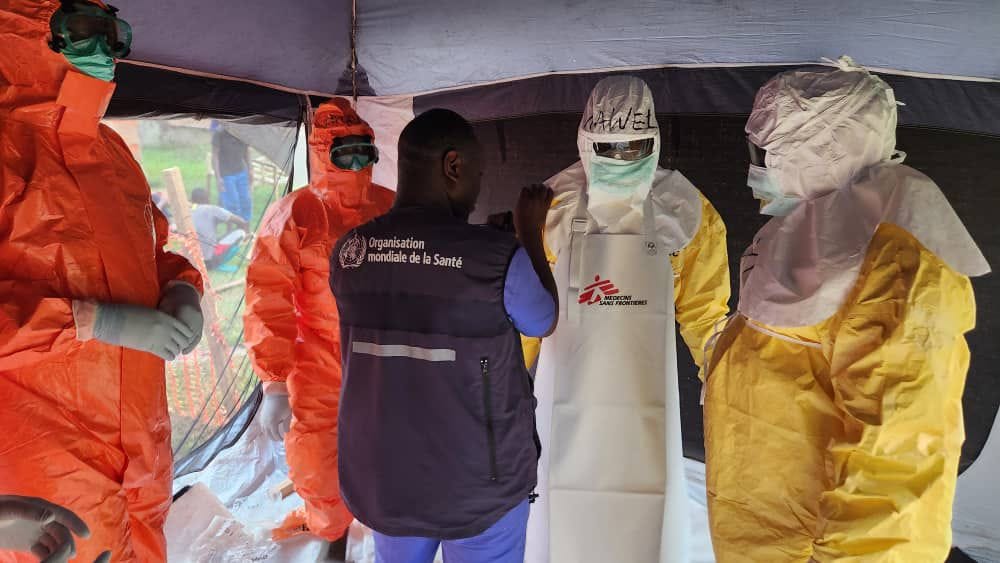
After laboratory testing at the National Public Health Laboratory (INRB) in Kinshasa confirmed the presence of the Ebola virus, a national Rapid Response Team supported by WHO experts in epidemiology, infection prevention and control, laboratory science, and case management was deployed to contain the outbreak and limit its spread.
To support the response, WHO allocated US$ 2 million from its Contingency Fund for Emergencies (CFE) in September 2025. The first disbursement of US$ 500,000 was to be directed to strengthen coordination, surveillance, and supply of basic protective equipment. This was followed by an additional US$ 1.5 million to expand laboratory capacity, risk communication, and community engagement.
WHO has delivered 12 tonnes of outbreak control materials and two tonnes of emergency health supplies to help manage the outbreak and protect health workers. Meanwhile, a stockpile of 2,000 doses of the Ervebo vaccine was already pre-positioned in Kinshasa, DRC, ready for deployment. This rapid financing mechanism, made possible through the Contingency Fund for Emergencies, established after the West Africa Ebola outbreak, reflects lessons learned from previous outbreaks and marks an improvement on past responses when delays in deploying resources accelerated virus transmission.
For now, the outbreak remains concentrated in Bulape and Mweka zones in Kasai Province, but these areas are difficult to access. Road travel from Kinshasa can take several days, causing significant delay in the movement of personnel, laboratory equipment, and medical supplies.
“The affected localities are hard to reach. We are working round the clock to rapidly roll out response measures to ensure robust outbreak control to stop the virus from spreading further and save lives”
~ Dr Mohamed Janabi, WHO Regional Director for Africa
Globally, past outbreaks have shown how fragile health systems, delayed funding, and weak community engagement can turn a small cluster of cases into a full blown epidemic, claiming many lives. Yet, recent responses suggest that lessons have been learned, with actions now implemented more rapidly. The great unknown, however, is the impact of declining foreign aid. The Kasai outbreak raises an urgent question:
What must African countries do differently now to avoid repeating the mistakes of the past?
The delayed response during the 2014–2016 outbreak allowed the virus to spread widely, resulting in more than 28,600 cases and 11,325 deaths. Human mobility across affected countries made contact tracing very difficult, while unsafe burial practices further worsened transmission. To prevent a repeat, African governments have prioritised community engagement, working with local communities, traditional leaders and faith-based organisations to build trust, educate people, counter misinformation, and promote safe culturally acceptable interventions for their communities.
African countries, both individually and collectively, need to develop rapid response mechanism for future outbreaks. This includes maintaining stockpiles of essential supplies, investing in local manufacturing of personal protective equipment (PPE), diagnostics, and ensuring the safety of the health workforce. This can be done through strong national public health agencies, with continuous training for health workers central to achieving this.
Why this matters
Ebola outbreaks are no longer uncommon in the Democratic Republic of Congo, and each one places additional strain on an already frail health system. Yet with every outbreak, the country’s capacity to respond has improved, supported by the country’s new national public health institute, l'Institut National de Santé Publique. Once the most recent outbreak was confirmed, the response was swift and highly coordinated. The Kasai outbreak really emphasises the urgent need for stronger preparedness, rapid access to vaccines and diagnostics, and sustained investment in local capacity. Until these gaps are addressed, every new case will continue to carry the risk of escalating into another regional, or even global crisis.